Dear Neighbors,
 For
many years, the work of caring for older people and young children has
faced an increasing crisis as there are just not enough people willing
to do the work for the low pay. The Boston Foundation's Boston
Indicators and Skillworks released an extremely important report on that workforce; last week, the Caucus of Women Legislators hosted a presentation on it. For
many years, the work of caring for older people and young children has
faced an increasing crisis as there are just not enough people willing
to do the work for the low pay. The Boston Foundation's Boston
Indicators and Skillworks released an extremely important report on that workforce; last week, the Caucus of Women Legislators hosted a presentation on it.
The report shows the historical roots of this problem and emphasizes the
injustice of undervaluing this work. It signals that the Boston
Foundation, with its credibility and influence, sees the issue as an
urgent one of racial and gender justice.
This newsletter is a shortish summary, along with ideas and information
from my work as chair of the Elder Affairs Committee. I hope you will
read the full report, and push for solutions to the problem of low wages and work shortage in these crucial - yes, essential - jobs.
Andre Green, Director of SkillWorks and
chair of the Somerville School Committee, introduced the report at the
Women's Caucus briefing. He has said, "If we paid jobs according to
their value to society, child care workers, home care workers and
long-term care workers would be at the top of the scale. But too often,
we determine our pay scales not by what the job is, but rather by who
does it. COVID underscored the essential nature of care work – the
question now is whether we are willing to acknowledge and value that
essential nature with higher pay and better working conditions.”
Historical Roots of Undervaluing Caregiving
Until the Industrial Revolution, care of
children and people with disabilities was mostly done by women at home.
Wealthy white women were able to perform culturally valued roles like
hostessing parties and directing servants, while laundry, cleaning, and
other "dirty work" were off-loaded onto enslaved Black women and other
lower class women.
As white women moved into the labor force in retail and clerical jobs,
women of color were "channeled into domestic labor." Labor reforms of
the twentieth century excluded most care workers. Home care workers were
only included in federal minimum wage and overtime protections in
2015; Massachusetts passed the Domestic Workers Bill of Rights just the
year before.
Increased Need for Workers
 People are living longer, and surviving longer with disabilities. US life expectancy rose from 47 years in 1900 to nearly 79 years in 2019 - though it has actually fallen since, and was 76 in 2021, due largely to COVID and opioid overdoses. People are living longer, and surviving longer with disabilities. US life expectancy rose from 47 years in 1900 to nearly 79 years in 2019 - though it has actually fallen since, and was 76 in 2021, due largely to COVID and opioid overdoses.
Not surprisingly, the need for careworkers is expanding. These are now the fastest-growing jobs in the workforce.
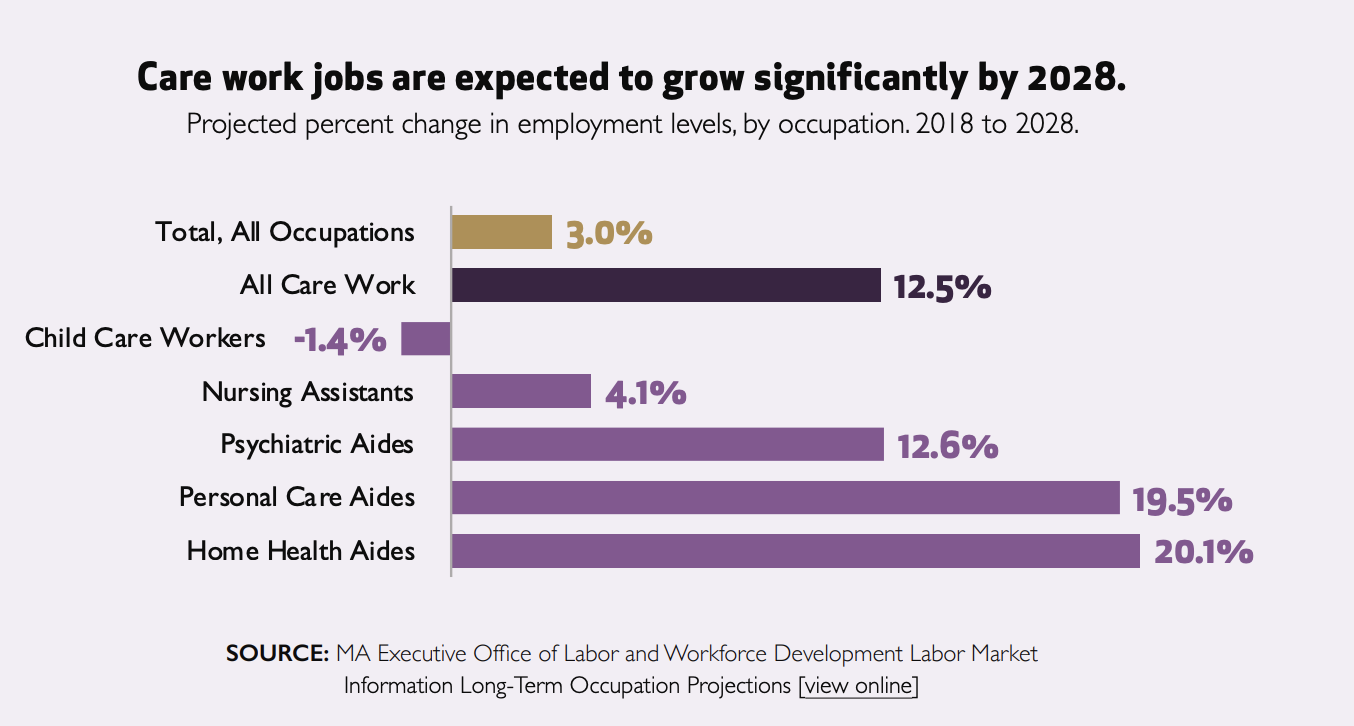
But home care agencies, nursing homes, and child care centers can't find
nearly enough workers to fill those jobs, which means many people
aren't receiving services they need, and families can't get the care
that would allow them to work.
The Effect of Worker Shortages
Right now, there are close to 5000 older people who qualify for public home care services, but who aren't receiving them because of a shortage of workers.
Right now, many hundreds of patients are in hospitals waiting to be discharged to nursing homes that can’t accept them because of staff shortages. Nursing homes report
a shortage of 6700 nursing positions and 1700 non-nursing positions.
As a result, more than half have limited their admissions.
19% of child care programs closed permanently during
the pandemic, Most remaining ones are short staffed and and almost a
quarter of them lack enough staff to enroll the number of children
they’re licensed to serve, according the the Mass. Department of Early Education and Care.
This is particularly true in centers that serve low income people and
families of color, so those parents have a harder time working.
Who are the Caregivers?
.
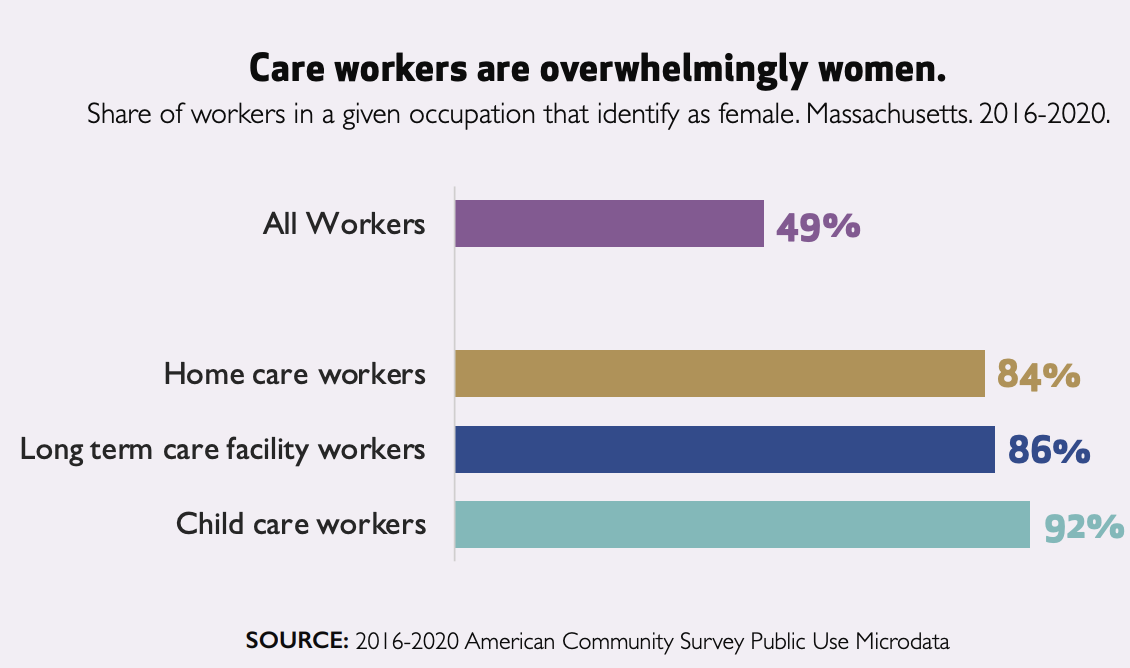
Caregivers are overwhelmingly women, and disproportionately people of color.
The report notes that "The vast overrepresentation of Black workers in
home care and long-term care facility work reflects the long history
described earlier of racial and gender discrimination that has relegated
Black women to the most physically taxing direct care."
Low pay causes shortages
 Direct care workers do crucial work, and were celebrated as essential workers during the early pandemic. But their wages are
near the bottom of all occupations. The chart shows that they earn a
little more than half the average hourly wage. The chart is for
2016-20; wages have gone up, especially due to the state minimum wage
increase as well as ARPA funds dedicated to temporary Medicaid rate
increases. Direct care workers do crucial work, and were celebrated as essential workers during the early pandemic. But their wages are
near the bottom of all occupations. The chart shows that they earn a
little more than half the average hourly wage. The chart is for
2016-20; wages have gone up, especially due to the state minimum wage
increase as well as ARPA funds dedicated to temporary Medicaid rate
increases.
Wages in nursing homes are now closer to $18 per hour.. Personal Care
Assistants (PCAs) in Massachusetts are unionized and recently bargained
for a minimum wage of $17.75. Pay increases have not kept up with
inflation, especially in housing
Due to the Grand Bargain of 2018, the MA minimum wage will increase to $15/hour in January. This is the last year of the phased increase to "Fight for Fifteen." Tipped employees' minimum employer pay will be only $6.75 and premium pay for Sundays and holidays will end. Farmworkers, fishermen, and
some other occupations are still not protected by overtime provisions.
Plenty of legislative work needed, as I've learned as chair of Labor
and Workforce Development.
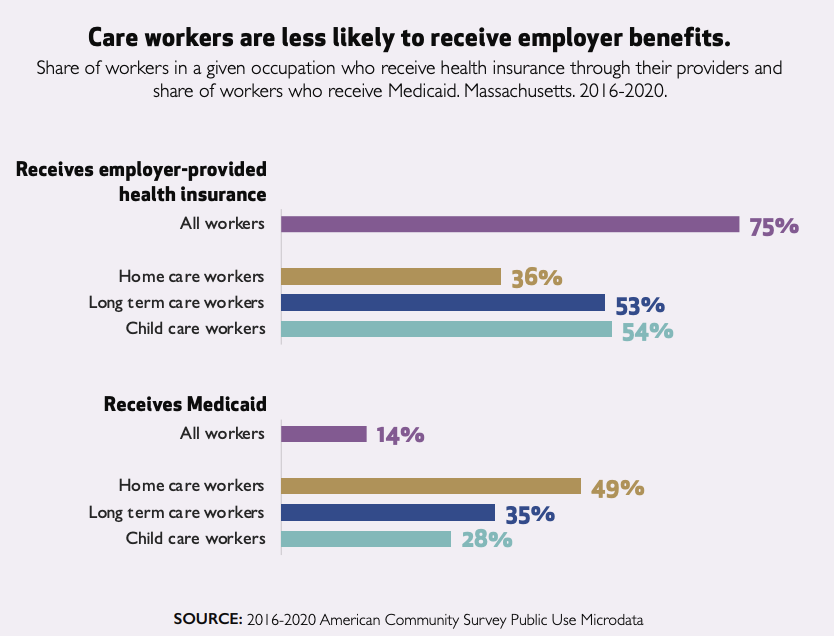 Careworkers
are also much less likely to receive employer-paid health insurance and
far more likely to rely on MassHealth (Medicaid). They are more likely
to qualify for SNAP (food stamp) benefits. This means that if they manage to work enough hours they will hit the cliff effect and lose benefits. Careworkers
are also much less likely to receive employer-paid health insurance and
far more likely to rely on MassHealth (Medicaid). They are more likely
to qualify for SNAP (food stamp) benefits. This means that if they manage to work enough hours they will hit the cliff effect and lose benefits.
They are also less likely to have pension plans: 35 percent of the total
workforce has a pension or other retirement plan (we all need one, even
with Social Security) compared to just 10.2% of child-care workers and
12.6% of home care workers. This means that the workers who are poor
now because they care for older people will be even poorer when they
themselves retire.
Poor job quality adds to shortage
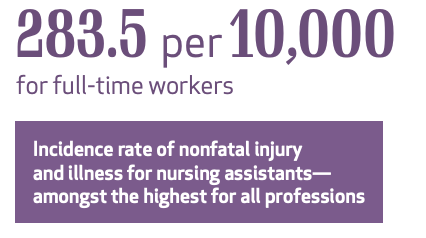 These
jobs are often very physically and emotionally stressful. Nursing
assistants have one of the highest injury rates of any job. Home care
workers have erratic schedules, and may not be paid if their client is
sick and cancels service. Having to care for several clients a day
means they may have unpaid travel time (despite the law) and are more likely to be exposed to COVID and other dangers. These
jobs are often very physically and emotionally stressful. Nursing
assistants have one of the highest injury rates of any job. Home care
workers have erratic schedules, and may not be paid if their client is
sick and cancels service. Having to care for several clients a day
means they may have unpaid travel time (despite the law) and are more likely to be exposed to COVID and other dangers.
Low pay and low job quality lead to high annual turnover
rates of over 30 percent in child care and up to 128 percent in nursing
home workers. Turnover, of course, means that workers have less
training and experience, and are less able to provide excellent care for
vulnerable people.
Reduced immigration adds to shortage
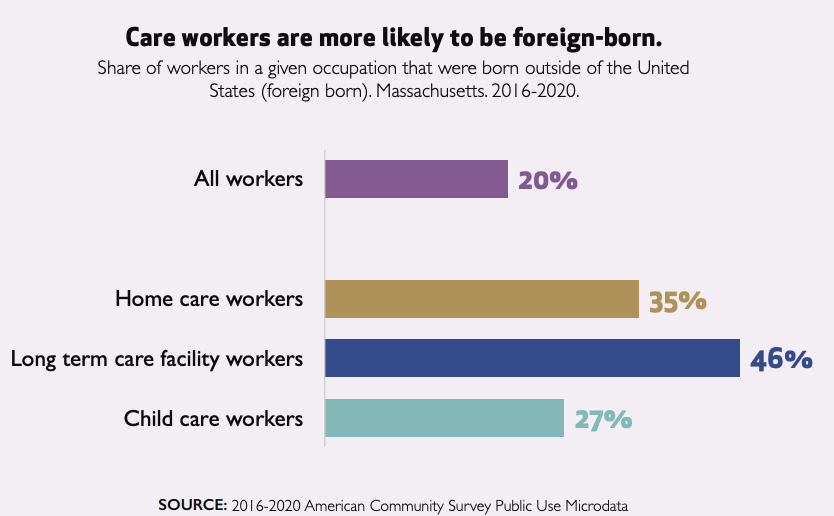 Caregivers
are more likely to be immigrants, including almost half of nursing home
workers. The report notes that "Immigrants, particularly immigrants of
color, drove Greater Boston’s population growth between 1990 and 2019,
accounting for almost 90 percent of net population change during that
period. Slowing immigration during the Trump administration combined
with international travel restrictions during the pandemic have led to
declining immigration rates in recent years." Caregivers
are more likely to be immigrants, including almost half of nursing home
workers. The report notes that "Immigrants, particularly immigrants of
color, drove Greater Boston’s population growth between 1990 and 2019,
accounting for almost 90 percent of net population change during that
period. Slowing immigration during the Trump administration combined
with international travel restrictions during the pandemic have led to
declining immigration rates in recent years."
Unpaid Caregivers Provide More Care
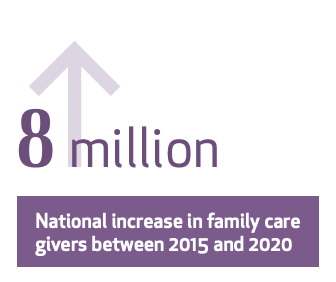 Family members provide many hours of unpaid care for both children and older people who need help. Mass. Caregivers Coalition
estimates that pre-pandemic there were 844,000 unpaid family members
caring for older relatives, of whom more than 600,000 were also
employed. Some of these people are part of the sandwich generation,
caring for parents and children at the same time. Family members provide many hours of unpaid care for both children and older people who need help. Mass. Caregivers Coalition
estimates that pre-pandemic there were 844,000 unpaid family members
caring for older relatives, of whom more than 600,000 were also
employed. Some of these people are part of the sandwich generation,
caring for parents and children at the same time.
As more people live longer and hope to age in place, these caregivers play an important role. Innovations such as "hospital at home"
offer many benefits but often require someone to be available to help.
But the cost in lost income and stress can be significant. The report
says that "affordable child care would lead to an increase of over
$100,000 in lifetime net income for Black mothers, the highest of any
racial or ethnic group."
Solutions?
The report recommends policy changes to improve care workers' job quality:
- continue to raise the minimum wage
- license home care agencies
- strengthen career ladders
- expand the Earned Income Tax Credit to unpaid family caregivers
- improve care workers' ability to unionize
We
can also provide free training and incentives to join this workforce.
An important reform Mass. Home Care and others have sought for years
would be to allow spouses to be paid as caregivers
by MassHealth. 15 other states allow this. This is one of many
proposals for long term care we hope the legislative leadership will
prioritize and the new Healey-Driscoll administration will embrace in
the new year. I am encouraged by the formation of Dignity Alliance Massachusetts, which brings together groups and advocates to push for more focus on the needs of older adults.
In
solving the crisis in caregiving, there is absolutely no substitute for
more money, and for higher pay. Since the state funds so much of the
nursing home, home care, and (less so) early care industry, it will take
a lot more of the state budget. It will mean, in my opinion, being
willing to ask the people and companies who have seen great increases in
their wealth to contribute more to build a more just economy and
society. Everyone, rich and poor and middle class, will benefit when
these essential workers are paid a fair wage, and there are enough of
them to serve all of us.
Stay safe and stay in touch,

|

0 comments:
Post a Comment